History of the Convergent Procedure
“We foresee that the combination of the two approaches (i.e., surgical and percutaneous approach), in common hybrid approach, will allow a substantial reform for the definitive cure of atrial fibrillation, …, providing the highest success rates along with the best care for patients' health.”
Bisleri G, Curnis A, Bottio T, et al, The Need of a Hybrid Approach for the Treatment of Atrial Fibrillation, The Heart Surgery Forum, 2005; 8 (5): E326 - E330 |
In the 1980’s pioneering surgeon Dr. James Cox began research into the creation of a surgical technique to treat atrial fibrillation. This research led to the Cox-maze procedure; the gold standard for the surgical treatment of atrial fibrillation. The Cox-maze provides for the definitive treatment of AF, but is a technically complex, open heart, on-bypass procedure that has made it a less then common procedure.
Improvements on the procedure led, through multiple variations, to the Cox-maze III and IV procedures that are more commonly done, but still invasive and with many of those complications associated with procedures requiring bypass.
Percutaneous Catheter-based ablation has become a viable treatment option for many cardiac arrhythmias. In fact, the only device approved for the treatment of AF in the United States is a catheter ablation device. Additionally, much of the technological advancement in catheter-based treatments has led to significant improvements in measurement, mapping and guidance abilities. It is now possible to merge a high-resolution X-ray image of the heart with electronic landmarks to create an extremely accurate map of the heart permitting targeted and accurate placement of catheter ablation devices. However, even with all of the technological improvements, Catheter Ablation still has a high ‘re-do’ rate and the first-time success rate is markedly variable.
The beginning of the Convergent Procedure
 In January, 2009, Dr. Andy Kiser and Dr. Mark Landers, from FirstHealth Moore Regional Hospital in Pinehurst, NC, assembled an international team of renowned Surgeons and Cardiologists in Krakow, Poland to explore new ways to treat Atrial Fibrillation. This team consisted of Dr. Rodney Horton and Dr. Andrew Hume from St. David’s Hospital in Austin, TX, Dr. David Haines from Beaumont Hospital in Detroit, MI, and Dr. Borut Gersak, Dr. Maiaz Sinkovec, and Dr. Andrej Pernat from University Medical Center in Ljubljana, Slovenia. They performed the first Convergent Procedure for Atrial Fibrillation, bringing together the expertise of Cardiac Surgeons and Electrophysiologists for the treatment of Atrial Fibrillation. In January, 2009, Dr. Andy Kiser and Dr. Mark Landers, from FirstHealth Moore Regional Hospital in Pinehurst, NC, assembled an international team of renowned Surgeons and Cardiologists in Krakow, Poland to explore new ways to treat Atrial Fibrillation. This team consisted of Dr. Rodney Horton and Dr. Andrew Hume from St. David’s Hospital in Austin, TX, Dr. David Haines from Beaumont Hospital in Detroit, MI, and Dr. Borut Gersak, Dr. Maiaz Sinkovec, and Dr. Andrej Pernat from University Medical Center in Ljubljana, Slovenia. They performed the first Convergent Procedure for Atrial Fibrillation, bringing together the expertise of Cardiac Surgeons and Electrophysiologists for the treatment of Atrial Fibrillation.
This Convergent Procedure allows doctors from different fields of medicine to work side-by-side to simultaneously treat Atrial Fibrillation, and now this procedure has been performed in the United States with the first patient treated at FirstHealth Moore Regional Hospital.
Until now, Catheter Ablation and Surgery were offered as part of the many treatment options for AF. Following the ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation 1, patients had few non-pharmacological choices; either endocardial ablation or some form of surgical procedure. Many of the medications for Atrial Fibrillation have significant side effects and frequently failed requiring moving from one drug to another. Now, with the convergent procedure, patients can have another option that offers the best treatment from all of the specialties, reducing many of the less desirable aspects.
The Ex-Maze procedure, pioneered by Dr. Kiser, offered a beating-heart, off-bypass surgical solution to patients with chronic AF.
 |
| Pictured (left to right) are Drs. Horton, Haines, Kiser, Bartus, and Hume performing the first convergent procedure in Krakow, Poland. Dr. Krzysztof Bartus and Prof. Jerzy Sadowski from the Jagiellonian University, Department of Cardiovascular Surgery and Transplantology in Krakow, Poland were instrumental in organizing the world’s first convergent procedure for atrial fibrillation. |
In an effort to further improve on the success of the Ex-Maze procedure, Dr. Kiser and a group of dedicated Cardiologists, Nurses and Physician Assistants have sought ways to reduce the less desirable aspects of the procedure, such as incisions in the chest.
Catheter Ablation has had significant improvements in recent years, but practitioners have sought ways to reduce the amount of radiation received and the time spent on the entire procedure.
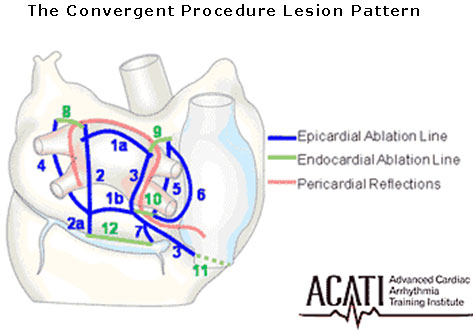
During the Convergent Procedure, the surgeons complete their part on the outside surface of the heart. Then the electrophysiologist make an electrical map of the inside of the heart to search for any residual areas which may require further treatment. The electrophysiologist uses a special ablation catheter placed in the large vein in the leg to perform their portion of the Convergent Procedure. They are then able to create additional lesions on the inside of the heart in locations that the surgeons are unable to reach without stopping the heart or cutting into the heart. These additional lesions further eliminate atrial fibrillation and prevent it from recurring.
This picture (below right) demonstrates the effectiveness of the Convergent procedure. The area in red is the posterior left atrium, the site where the majority of triggers for atrial fibrillation are located. The red color indicates that this area has little, if any, residual electrical activity. This demonstrates the elimination of the electrical problems that cause atrial fibrillation.
|
| This picture demonstrates the effectiveness of the Convergent procedure. The area in red is the posterior left atium atrium, the site where the majority of triggers for atrial fibrillation are located. The red color indicates that this area has little, if any, residual electrical activity. This demonstrates the elimination of the electrical problems which cause atrial fibrillation. |
Electrophysiologic Studies (EPS) and intra-cardiac mapping clearly demonstrate the effectiveness of the Convergent procedure. This allows for less procedure time and less fluoroscopy (radiation) exposure during catheter ablation. For the surgeon, the Convergent Procedure reduces the overall operative time, avoids chest incisions and lung deflation, and uses only three miniature abdominal incisions in addition to the access for the catheter ablation.
For the patient, it means less pain, smaller scars and offers a shorter hospital stay and a greater overall procedural success.
View the American Heart Association Catheter Ablation Web Page
1 Fuster V, Rydén LE, Cannom DS, et al, ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation). Circulation. 2006;114:e257-e354
|