Advantages of the Convergent Procedure
 Advantages of the Convergent Procedure Advantages of the Convergent Procedure
Andy C. Kiser, M.D.
Clinical Assistant Professor of Surgery, East Carolina University
Director, FirstHealth Arrhythmia Center/ACATI
Pinehurst, NC, US
Cardiac surgeons continually strive toward less invasive procedures which avoid approaches like full median sternotomies and thoracotomies. However, reports of “minimally invasive” cardiac surgical procedures may include hemi-sternotomies, “mini-thoracotomies”, or full median sternotomies without cardiopulmonary bypass.
True minimally invasive procedures must not only be defined by the size of the incision, but also by the invasiveness into the patient’s daily lifestyle and the impact on their quality of life.
There are a variety of techniques and devices in use for the surgical treatment of atrial fibrillation (AF). The current ‘gold standard’ for the surgical treatment has been the Cox “cut and sew” maze procedure. There have been variations through the years leading to a host of other surgical AF procedures, such as the Wolf mini-maze1, practiced by many surgeons. Other techniques create myocardial lesions using some form of radiofrequency energy, laser, cryothermy or high-frequency ultrasound. All of these techniques require access to the heart through either a full sternotomy or less-invasive approaches with incisions on the left and/or right side of the chest. Some techniques require cardiopulmonary bypass and sometimes cardioplegia to stop the heart entirely2,3. Until recently, no current technique or device provided access to the posterior left atrium directly.
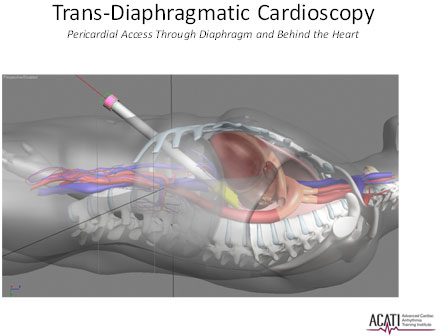
Cardioscopy is a totally endoscopic technique that provides direct visualization of, and access to, the epicardial surface of the beating heart without the need for cardiopulmonary bypass or prolonged postoperative recovery. Unlike a subxyphoid approach, Cardioscopy provides access to the heart via the central tendon of the diaphragm. This allows direct vision of the posterior cardiac structures with minimal hemodynamic compromise. Such access and visualization of the epicardial cardiac surface has enabled epicardial ablation techniques, like the Convergent Procedure, as a treatment for atrial fibrillation4,5. Cardioscopy eliminates the need for sternotomy or thoracotomy when access to the epicardial surface is necessary.
The Convergent Procedure: Simultaneous Endocardial and Epicardial Ablation
The surgical treatment of atrial fibrillation (AF) is based upon the creation of an anatomical pattern of myocardial scar. The Corridor procedure6, the Radial Maze Procedure7, and the Cox maze I-III8,9, are anatomical patterns designed to disrupt the re-entry circuits of AF by dividing the atria into non-conductive segments. Electrophysiologists, in comparison, use endocardial catheters and electrodes to identify the triggers causing AF and direct their treatments towards these foci of abnormal electrical activity in the atria. The individual success of these approaches, either surgical or endocardial, has been limited by technical complexity and/or less than desirable outcomes.
A truly successful and adoptable AF treatment has always seemed to be “just out of reach”. The acclaimed “gold standard” cut and sew maze procedure reports exceptional outcomes but remains a complex procedure that is rarely performed10,11. The “mini-maze”1 and pulmonary vein isolation12 reduce procedural complexity by decreasing the number of lesions and by eliminating cardiopulmonary bypass. However, both the surgeons and the cardiologists have demonstrated that when treatment is limited to the left atrium, outcomes suffer as a consequence13,14. The endocardial, catheter-based AF ablations, not unlike the surgical procedures, remain long and technically difficult procedures performed by relatively few electrophysiologists. The high rate of repeat procedures and less than desirable long-term outcomes have been disappointing15. Unfortunately, surgeons and cardiologists seldom collaborate in the development of new technologies and innovative approaches to overcome these individual procedural shortcomings.
The Convergent Procedure has been developed by a multidisciplinary team of cardiologist and cardiac surgeons to address the procedural and communication barriers. The Convergent procedure is the simultaneous creation of a surgeon’s PEX epicardial ablation pattern and electrophysiologist’s endocardial ablation pattern (Figure 1).

Figure 1. The Convergent Procedure Lesion Pattern
The surgeon’s ability to effectively create visible, and therefore contiguous, epicardial ablation lines has greatly reduced the amount of endocardial tissue which must be ablated to complete a successful trans-septal catheter procedure. The integration of a surgeon’s anatomical approach to AF with the physiological approach of the electrophysiologist’s has led to the development of the Convergent procedure.
This convergence of technologies and expertise provides or allows for:
- the creation of a complete, bi-atrial, endocardial and epicardial ablation pattern without a chest incision or cardiopulmonary bypass;
- intra-operative metrics to confirm procedural success;
- integrated patient care by cardiology and cardiac surgery; and
- decreased length of hospital stay and the number of repeat ablation procedures.
An Integrated Approach to the AF Patient
At FirstHealth Moore Regional Hospital, we have created a multidisciplinary service that integrates the care of Arrhythmia patients. Evaluation of each case by the multidisciplinary team of arrhythmia experts ensures an individualized, yet consensus, treatment plan. Without this integrated approach, the best treatment option may not be available or may require much longer wait times, more travel and more inconvenience and delay for the patient.
The patient’s clinical presentation is vitally important to developing the multidisciplinary treatment plan. Left atrial size, AF type and AF duration are significant contributory factors. We advocate a 24-hour Holter monitor on all patients under evaluation to document the degree of AF burden. Additional evaluation includes a trans-thoracic echocardiogram and cardiac catheterization or stress test to exclude structural heart disease in the setting of AF. We have anecdotally discovered associated structural heart disease in 30%-45% of the population presenting for stand-alone AF treatment.
The consensus opinion by the Heart Rhythm Society Task Force states that “Stand-alone AF surgery should be considered for symptomatic AF patients who prefer a surgical approach, have failed one or more attempts at catheter ablation, or are not candidates for catheter ablation.” Left atrial size and AF duration are important factors in this decision process. When the left atrium is larger than 6.0 cm or the duration of AF is greater than 5 years, the long term success for the “Cut and Sew” maze procedure are under 80% (Figure 2). It is difficult for the electrophysiologist to consistently and effectively complete pulmonary vein isolation when the left atrium is greater than 5.0 cm. Therefore, when a patient has paroxysmal AF and the left atrium is under 4.5-5.0 cm, we recommend percutaneous catheter ablation. In this population, simple pulmonary vein isolation may be effective in over 80% of patients16.
Patients with paroxysmal AF and a left atrium greater than 4.5 cm and those with persistent and long-standing persistent AF demonstrate the best outcomes when a bi-atrial lesion pattern is created. Surgeons who have experience with minimally invasive approaches choose the ablation technology best suited for their technique. Whichever approach and device is used, a comprehensive lesion pattern of contiguous and transmural lesions are essential. Persistence and intra-operative verification of lesion and pattern integrity is crucial. The Convergent Procedure has established new criteria for lesion integrity by the verification of procedural completion by endocardial electrophysiologic metrics. The Convergent Procedure is not complete until pulmonary vein isolation and posterior left atrial exclusion is confirmed, the coronary sinus is ablated, and a cavo-tricuspid isthmus lesion is created. These metrics provide confidence of procedural success and set new standards for the hybrid treatment of persistent and long-standing persistent AF.
Conclusion
There have been many minimally invasive approaches to treat AF, all based primarily upon the original work by Cox and his Maze procedure. By integrating electrophysiology and cardiac surgery in a “hybrid” AF treatment, new procedural and perioperative standards have been established at our institution. The initial outcomes utilizing this multidisciplinary approach are excellent and patient satisfaction is overwhelmingly positive.
1Wolf RK, Schneeberger EW, Osterday R, Miller D, Merrill W, Flege JB Jr, Gillinov AM. Video-assisted bilateral pulmonary vein isolation and left atrial appendage exclusion for atrial fibrillation. J Thorac Cardiovasc Surg. 2005; 130:797-802
2Henry L, Ad N. The Maze procedure: a surgical intervention for ablation of atrial fibrillation. Heart Lung. 2008 Nov-Dec;37(6):432-9.
3Chitwood WR Jr, Wixon CL, Elbeery JR, Moran JF, Chapman WH, Lust RM., Video-assisted minimally invasive mitral valve surgery, J Thorac Cardiovasc Surg. 1997 Nov;114(5):773-80; discussion 780-2
4Kiser AC, Wimmer-Greinecker G, Chitwood WR. Totally extracardiac maze procedure performed on the beating heart. Ann Thorac Surg 2007;84:1783-85
5Kiser AC, Wimmer-Greinecker G, Kapelak B, Bartus K, Sadowski J. Paracardioscopic ex-maze procedure for atrial fibrillation. Innovations 2008; 3:117.
6Defauw JJ, Guiraudon GM, van Hemel NM, Vermeulen FE, Kingma JH, de Bakker JM. Surgical therapy of paroxysmal atrial fibrillation with the "corridor" operation. Ann Thorac Surg. 1992; 53(4):564-70.
7Nitta T, Lee R, Schuessler RB, Boineau JP, Cox JL. Radial approach: a new concept in surgical treatment for atrial fibrillation I. Concept, anatomic and physiologic bases and development of a procedure. Ann Thorac Surg. 1999 Jan;67(1):27-35.2
8Cox JL, Schuessler RB, D'Agostino HJ Jr, et al.The surgical treatment of atrial fibrillation. III. Development of a definitive surgical procedure. J Thorac Cardiovasc Surg. 1991 Apr;101(4):569-83.
9Cox JL, Boineau JP, Schuessler RB, et al. Modification of the Maze procedure for atrial flutter and atrial fibrillation: I. Rationale and surgical results. J Thorac and Cardiovasc Surg 1995; 110:485-495.
10Prasad SM, Maniar HS, Camillo CJ, et al. The Cox maze III procedure for atrial fibrillation: long-term efficacy in patients undergoing lone versus concomitant procedures. J Thorac Cardiovasc Surg. 2003; 126(6):1822-8.
11Kosakai Y. Treatment of atrial fibrillation using the maze procedure: the Japanese experience. Sem Thor Cardiovasc Surg. 2000; 12:44-52.
12Edgerton JR, Edgerton ZJ, Weaver T, et al. Minimally Invasive Pulmonary Vein Isolation and Partial Autonomic Denervation for Surgical Treatment of Atrial Fibrillation. Ann. Thorac. Surg. July 2008; 86:35-39.
13Barnett SD, Ad N. Surgical ablation as treatment for the elimination of atrial fibrillation: a meta-analysis. J Thorac Cardiovasc Surg. 2006 May;131(5):1029-35.
14Calo I, Lamberti F, Loricchio ML, et al. Left atrial ablation versus biatrial ablation for persistent and permanent atrial fibrillation: a prospective and randomized study. J Am Coll Cardiol 2006;47:2504-2512.
15Cappato R, Calkins H, Chen SA, et al. Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. 2005;111:1100-1105.
16Haissaguerre M, Jais P, Shah DC, Takahashi A, et al. Spontaneous initiation of atiral fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998; 339:659-666. |



